SingaporeMotherhood | Baby & Toddler
March 2024
Snoring? Insomnia? Daytime Fatigue? Your Child could have Sleep Disorders

Does your child sleep well? Children need sleep. But even more importantly, they need to sleep well. Sleep is crucial for their overall health and development, and plays a pivotal role in their cognitive functioning, emotional regulation, and physical growth. However, sleep disorders can significantly impact children’s well-being, leading to behavioural problems, mood disturbances, and concentration difficulties. Conditions such as insomnia and sleep apnoea can disrupt sleep patterns, causing daytime sleepiness and impairing cognitive function.
Therefore, fostering healthy sleep habits and addressing sleep disorders are crucial for promoting the optimal growth and development of young children. Ahead of World Sleep Day tomorrow (15 March 2024), we ask two doctor experts how to resolve sleep problems in children, and help our little ones get the best sleep of their lives.
(See also: BEDWETTING AND NIGHT TERRORS: ARE THESE SLEEP DISORDERS DISRUPTING YOUR CHILD’S NIGHTS?)
Featured doctors
(A) Sleep Disorders in General
What are the main sleep disorders that children have?
Dr Jenny
Paediatric sleep disorders vary with the age of children. Behavioural insomnia of childhood (including sleep onset association disorder and limit setting disorder) tends to start in early infancy and the toddler years. Parasomnias including night terror, confusional arousal, sleepwalking and obstructive sleep apnoea (OSA) tend to occur in toddlers and older children.
School-going children often experience less sleep than what they need due to school-related pressure and family schedules. This may lead to chronic sleep insufficiency. It is also often seen in adolescents who experience a shift to later bedtimes as a result of physiological changes in their body clock, school-related demands, and family and social pressures as well as use of electronic devices.
Dr Annette
A very common sleep disorder is associated with snoring and obstructive sleep apnoea (OSA), otherwise known as sleep-disordered breathing (SBD).
Snoring is caused by the vibration of tissues in the throat, It can be a symptom of partial airway obstruction. Such an obstruction can evolve into complete airway obstruction, leading to OSA. When the upper airway is obstructed, the oxygen supply to the brain, heart and vital organs is reduced. Over an extended period of time, this may result in other medical complications, such as heart disease and stroke. Snoring is sometimes accompanied by mouth breathing. As a child’s jaw grows and develops, such prolonged mouth breathing may result in an open bite.
Are these sleep disorders more common in Singapore?
Dr Jenny
According to studies, such sleep problems are highly common amongst children and adolescents, with prevalence rates ranging from 25% to 40%. The prevalence of these problems is even higher amongst certain populations, such as children ADHD and Down syndrome, where more than 80% may suffer from sleep disturbances. The prevalence amongst children in Singapore is estimated to be similar. The estimated OSA prevalence rate amongst children in Singapore is about 3%.
How do I know if my child has a sleep disorder?
Dr Jenny
Look out for habitual snoring, frequent arousals from sleep, difficulty in falling asleep or waking up, and paroxysmal events in sleep such as night terrors, sleep walking and head banging.
In addition, check if your child has daytime symptoms which are usually related to insufficient or poor quality of sleep. Examples include:
- Εxcessive daytime sleepiness
- Fatigue, lethargy and complaints about their body
- Inability to control mood and behaviour (e.g., irritability, anger tantrums, hyperactivity and inattention)
- Impairment of cognition and vigilance
- Declining performance in school, sports or games
- Compromised immune system and appetites
Dr Annette
Children with sleep disorders may snore while sleeping or use the mouth to breathe when sleeping. They may complain of fatigue or be excessively sleepy in the daytime despite having eight to nine hours of sleep. Some children complain of morning headaches or have problems staying focused in the classroom. This affects their performance in school.

How are such sleep disorders treated in children?
Dr Jenny
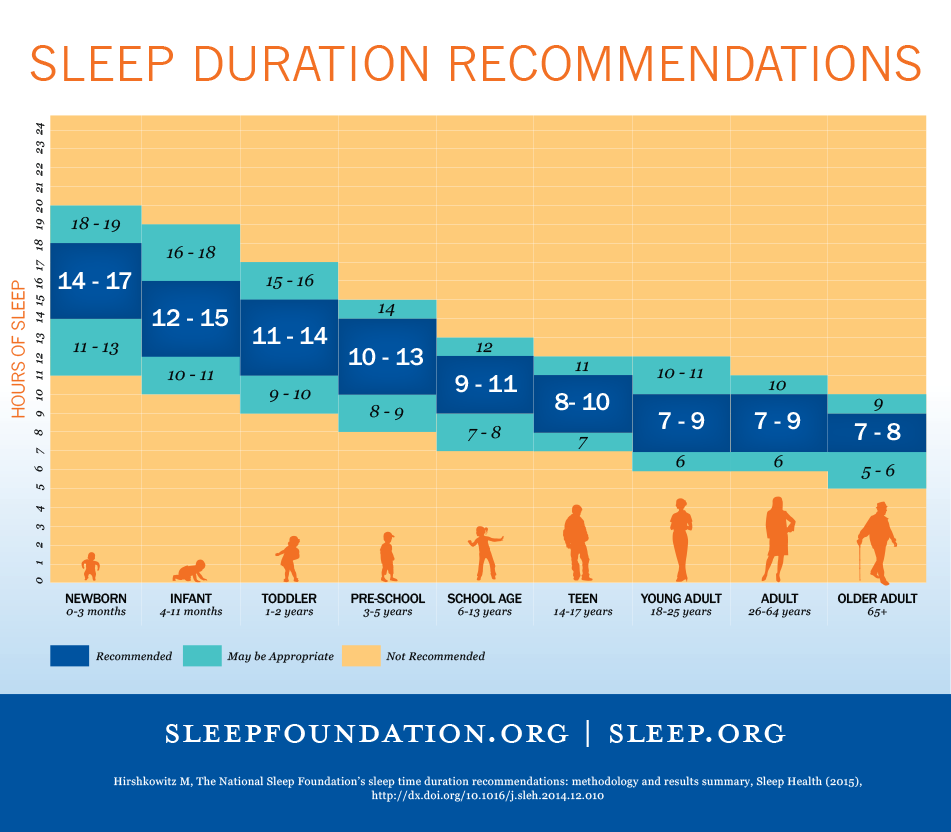
Prevention is the key. Failing this early diagnosis and intervention can minimise consequences. Parents and caregivers, including nannies, grandparents, school teachers and older children, should be made aware of the crucial elements of sleep i.e., importance and function of sleep, average sleep duration based on age, good sleep hygiene, prevention of sleep onset associations, as well as learn to recognise the signs and symptoms of common sleep problems. If parents have concerns or questions in this area, they should bring their children to seek early medical attention.
Dr Annette
Establishing a strict bedtime routine is a good start. The recommended daily routine should exclude the use of screen-based devices for at least an hour before bedtime, allow at least nine hours of sleep, and ensure a dark and cool bedroom setting.
(See also: BABY SLEEP SECRETS: TRAVELLING WITH BABY)
What are the available treatments for sleep disorders in children?
Dr Jenny
First of all, it is crucial for all children to adopt healthy sleep habits. Here are some tips from a book on common sleep disorders that I co-authored: Sleep medicine : a clinical guide to common sleep disorders.
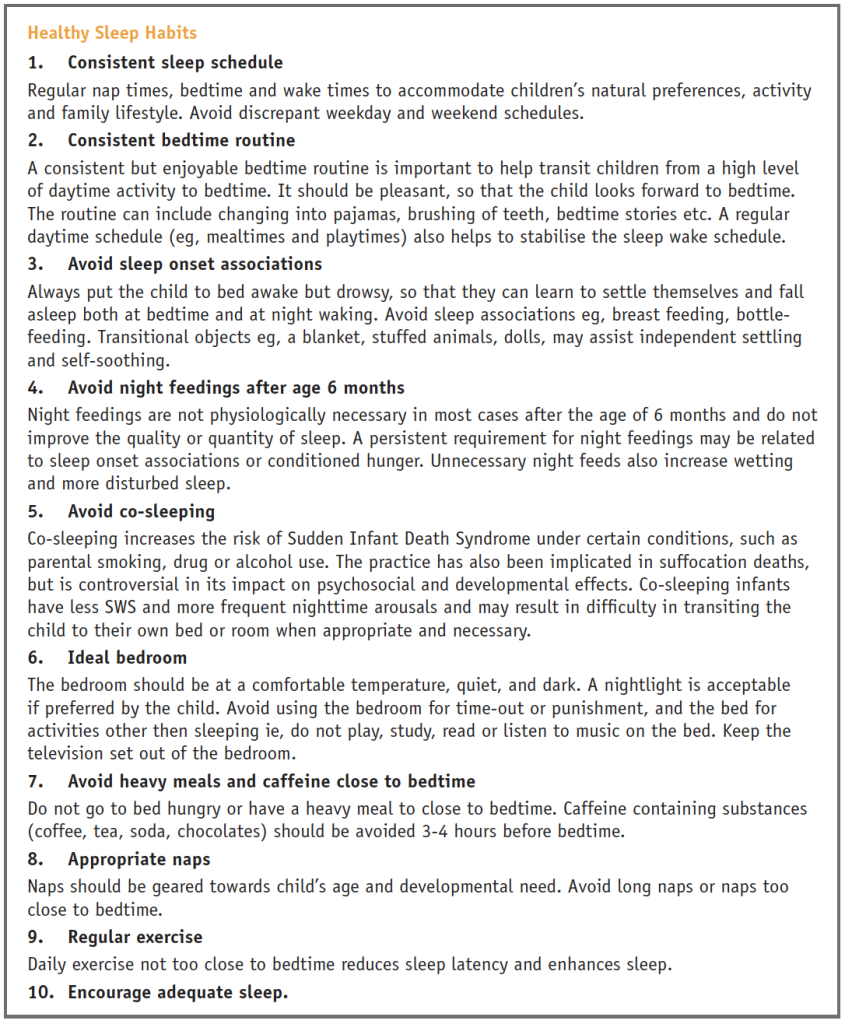
In addition, children could follow the average recommended sleep duration in the chart that is based on age (see below).
Other advice would be specific to the disorder in question. Here are some examples:
Childhood behavioural insomnia:
Sleep-onset association disorders
It is advisable for the child to be left in the cot drowsy but still awake. Give the child a “lovey” such as a stuffed toy or a used shirt from the mother. When your child is learning to fall asleep on his or her own, look at increasing the intervals between comforting your child (graduated extinction), until your child is able to fall asleep on his or her own. Another way is to put your child to bed at a designated time and ignore them until a set time the following morning (extinction).
Limit setting disorder
- Establish clear bedtime rules such as staying in bed and not calling out for parents
- Stick strictly to the set bedtime rules
- Ignore complaints about bedtime such as “I am not tired’
- Put your child to bed sleepy but awake
- Check on your child very briefly if needed, to provide reassurance and also to reinforce limits
- Return your child to bed immediately if they leave their bed
- Be consistent and firm between different caregivers
- Use positive reinforcement such as sticker charts
- Expect a temporary worsening of behaviour in the beginning of the programme before seeing significant improvement
(See also: THE ULTIMATE GUIDE TO ALL YOUR BABY SLEEP QUESTIONS, ANSWERED BY A SLEEP EXPERT)
(B) Sleep apnoea
What are the symptoms of sleep apnoea in a child?
Dr Jenny
Potential symptoms include:
Night time
- Snoring
- Restless sleep
- Unusual sleeping positions
- Increased work of breathing
- Witnessed apnoea
- Gasping and choking
- Excessive sweating
- Bedwetting
- Blueness and fits

Daytime
- Morning headaches
- Excessive daytime sleepiness and tiredness
- Behavioural concerns such as inattention, hyperactivity, emotional outbursts and anger tantrums
- Developmental delay
- Learning difficulties
- Growth disturbances
Dr Annette
A child with obstructive sleep apnoea (OSA) may experience the following:
- Snoring
- Excessive daytime sleepiness despite a good eight- to nine-hour sleep period
- Choking or gasping episodes during sleep
- Hyperactivity in the daytime
- Poor academic performance
- Morning headaches
(See also: WHEN YOUR CHILD HAS A HEADACHE)
Can children be put through sleep apnoea tests?
Dr Jenny
A formal evaluation of sleep apnoea in children is usually conducted through an attended overnight sleep study or Polysomnography (PSG). Such tests involve recording the child’s sleep for one night including brain waves, muscle movements, eye movements, breathing, snoring, oxygen and carbon dioxide levels, heart rate and leg movements. This assessment method is the gold standard and designed to be non-invasive and painless.
In the event that a PSG cannot be conducted, overnight recording of oxygen levels can be used as a less sensitive method for diagnosis.
Dr Annette
If a child snores persistently, the parent should bring him or her for review by an ear, nose and throat (ENT) surgeon. The child would be put through a comprehensive examination including an in-office nasoendoscopy (nasal endoscopy) to assess the anatomy of the upper airway. To further evaluate the child’s sleep dynamics, the doctor may recommend a sleep study or polysomnography.
Will a child with healthy sleeping habits develop sleep apnoea in adulthood?
Dr Jenny
It is possible. We also see sleep apnoea in adolescents and adults where obesity, allergies, smoking and family history of the same disorder are common contributing factors.
Dr Annette
Yes. When children grow and are exposed to childhood infections and environmental allergens, their adenoids and tonsils may enlarge with time. If the children put on excessive weight in a later part of their childhood, they are also predisposed to OSA.
(See also: 8 EXPERT STRATEGIES TO BUILD YOUR CHILD’S SELF-ESTEEM AND GIVE THEM CONFIDENCE IN LIFE)
How is sleep apnoea treated?
Dr Jenny
Treatment options will depend on contributing factors and if there is a co-existing disease. Some options include removal of tonsils and adenoids, Continuous Positive Airway Pressure (CPAP) therapy, orthodontic devices, myofunctional therapy, weight management, treatment of associated medical conditions such as reflux, allergies, asthma, and avoiding passive smoking.
Dr Annette
Our first approach to our paediatric patients is always to manage the condition with medications before we consider surgical means.
Most snoring children have underlying untreated or poorly treated allergic rhinitis. A treatment plan could be used to maximise the child’s clinical response to allergic rhinitis. This may involve household measures such as laundering bed linens and pyjamas fortnightly at 60°C and above to ensure house dust mites are killed, using an air purifier with a HEPA filter, removing all carpets and rugs in a child’s room, and maintaining the air conditioner regularly. Intranasal steroids, oral antihistamines and other medications may also be used.

In general, children experience upper airway obstruction due to excessive enlargement of the tonsils and adenoids. For such cases, surgery to remove the adenoids and tonsils will resolve the symptoms and give the child better sleep outcomes.
Other more complex surgeries include tracheostomy, palate surgery, tongue base surgery and remodelling of the facial skeleton. However, these surgical methods are rarely employed in children.
Weight loss measures are sometimes recommended if the child is likely to benefit.
Continuous Positive Airway Pressure (CPAP) could be used to apply air pressure to the narrow upper airway, similar to the way air is blown continuously into a bouncy castle! This allows it to maintain its shape, which is pivotal for oxygen transfer. Such a treatment plan is administered by a paediatric sleep physician in consultation with an ENT surgeon and is done via a face mask and special machine at the child’s bedside.
Is sleep apnoea a chronic lifetime sleep disorder?
Dr Jenny
Many children with mild OSA do get better with ‘watchful waiting’ and medical management of comorbid disease(s), such as allergies and asthma, that improve with time. About 40% to 70% of children who undergo surgery for OSA recover from the disease.
Children who have persistent risk factors such as obesity, nerve or muscle problems, or a positive family history of OSA are more likely to suffer from it in the longer term. Those who have been treated and recovered through means such as surgery continue to be at a higher risk of OSA in later childhood and adult years, but many will remain well.
Dr Annette
As mentioned above, if the cause of a child’s OSA is enlarged adenoids and tonsils, removing these soft tissue structures will resolve the child’s symptoms and improve long-term sleep and learning outcomes for the child.

What is the recommended sleeping position for a child with sleep apnoea?
Dr Jenny
Sleeping on the side or in the prone position usually reduces the severity of the sleep apnoea. Another way is to sleep with the neck extended as it optimises the open airway during sleep.
Dr Annette
In general, most children with OSA find it difficult to sleep in a supine position. They would be more comfortable in a side-sleeping position.
Will sleep apnoea negatively impact a child’s behaviour?
Dr Jenny
It is quite common for sleep apnoea to lead to daytime behavioural changes. Visible changes include excessive daytime sleepiness, tiredness, inattention, hyperactivity, impulsivity, emotional outbursts and anger tantrums. Many children thought to have possible ADHD and later found to have OSA drop the ADHD diagnosis after their OSA is treated.
Dr Annette
According to studies, OSA presents a huge economic burden to society. Individuals with untreated OSA are associated with poor work performances, occupational injuries and are involved in road traffic accidents more often.
In children, sleep disorders such as OSA can lead to poorer academic and extracurricular performances. Some children may be perceived as difficult to manage or as “having a temper” when they are in fact exhibiting poorer executive function due to a chronic lack of quality sleep.
(See also: BEDWETTING AND NIGHT TERRORS: ARE THESE SLEEP DISORDERS DISRUPTING YOUR CHILD’S NIGHTS?)
Featured image: pvproductions on Freepik
All content from this article, including images, cannot be reproduced without credits or written permission from SingaporeMotherhood.
Follow us on Facebook, Instagram, and Telegram for the latest article and promotion updates.





