SingaporeMotherhood | Baby & Toddler
December 2023
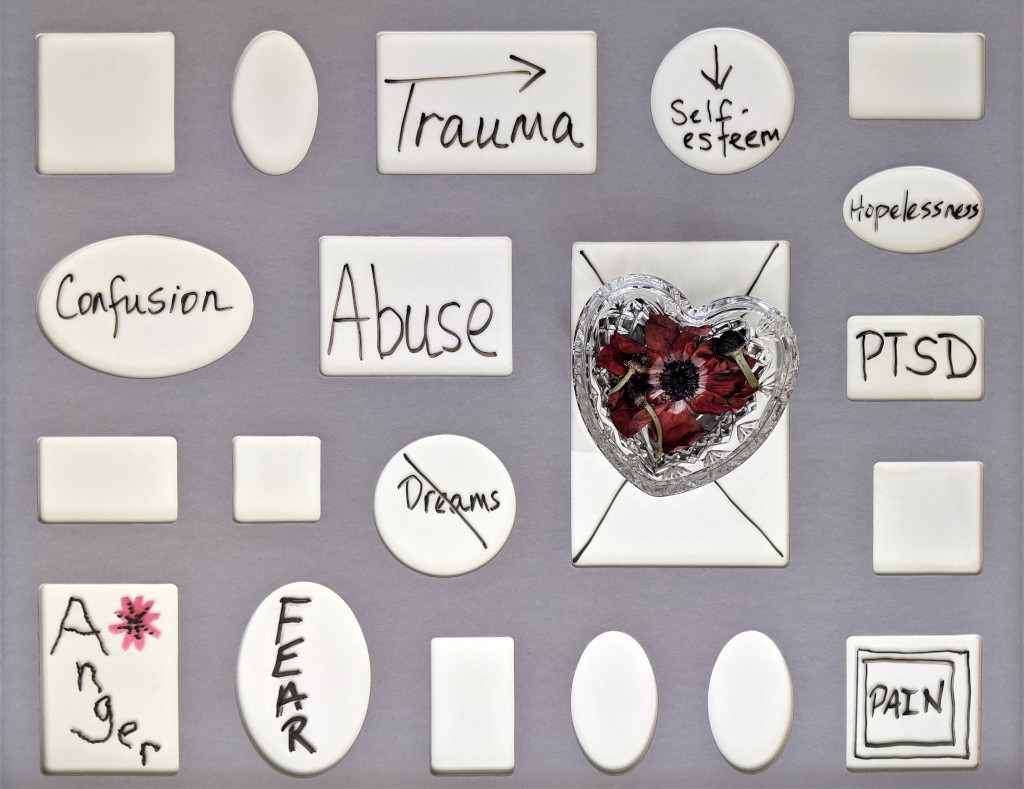
Postpartum Depression 101 – Beyond the Baby Blues

One of the most beautiful moments of human existence is when a mother brings life into the world. But such moments of joy can also lead to darkness. It is normal to experience post-birth blues and anxiety about this new, tiny person that you’re responsible for. However, there is a stark difference between that and something more serious, such as Postpartum Depression.
Recent data from KK Women’s and Children’s Hospital (KKH) indicates a staggering 47 per cent increase in Postpartum Depression cases between April 2021 and March 2022. Made worse by the COVID-19 pandemic, this surge in cases reveals the need for heightened public awareness. Also, the availability of support systems for both young and mature mothers who are equally susceptible.
Founder and director of Olive Branch Psychology and Therapy Clinic, Sam Roberts is a counsellor with over a decade’s worth of experience. He delves into the complexities of Postpartum Depression, a pervasive yet often misunderstood mental health condition that affects new mothers.
(See also: CRYSTALS HELPED THIS MUM HEAL FROM DEPRESSION. NOW SHE HELPS OTHERS WITH THEM)
What is Postpartum Depression?
Postpartum Depression (PPD) is a severe and persistent form of mood disorder. It can begin within the first few weeks after childbirth but may develop anytime in the first year. Symptoms include intense and prolonged feelings of sadness, hopelessness, and a loss of interest in daily activities. PPD can interfere with a mother’s ability to care for herself and her baby. It can also have a significant impact on the family.
A new mother may experience elements of mood fluctuations and some of these conditions are different but can also overlap. For example, Postpartum Anxiety is a condition that focuses more on excessive worry, irrational fears, and anxiety. Symptoms include racing thoughts, restlessness, and constant worrying about the baby’s health or safety. This can occur alongside or independently of PPD.

It’s just a phase, right?
PPD is not a phase that women naturally ‘get over’, but rather, a medical condition that requires serious attention and treatment.
It is important to recognise and address these conditions. Otherwise, it can significantly impact the mother’s emotional and physical well-being. Prolonged emotional distress doesn’t just affect overall health, but normal functioning on a day-to-day basis will become harder. It may even affect a mother’s ability to care for herself.
Furthermore, she may struggle to bond with or care for her baby, which can have long-term consequences on the child’s emotional and cognitive development. If not addressed well, it can also strain the relationship with the spouse and other family members. Of course, this could potentially lead to even more conflict and stress — a vicious cycle.
(See also: PARENTAL STRESS, ANXIETY, AND BURNOUT: ARE THEY HAPPENING TO YOU?)
Causes of Postpartum Depression
PPD is a complex condition and the exact cause of it is not fully understood. However, each woman’s experience with PPD is unique, and it is likely a combination of factors that contribute to it. Here are some factors for consideration:
Hormonal Changes: There are hormonal fluctuations that occur during pregnancy and childbirth. Changes in oestrogen and progesterone levels may play a crucial role. These affect brain chemistry, which can contribute to mood swings.
Biochemical Factors: Imbalances in certain neurotransmitters, such as serotonin and dopamine. These are involved in mood regulation, so they can also trigger emotional instability.
Physical Health: Physical health problems, either during or after pregnancy, can be a contributing factor. This might include complications during childbirth, chronic health conditions, or sleep disturbances.
Psychological Factors: Various psychological factors, including a history of depression or other mental health issues. High levels of stress, low self-esteem, as well as a lack of a healthy support system can influence mood irregularities.
Stressful Life Events: Life stressors, such as financial difficulties, relationship problems, or a traumatic birth experience can contribute to the onset of PPD.
Social and Cultural Factors: Social isolation, lack of a strong support system, cultural expectations, and societal pressures can all impact a woman’s risk of developing PPD.
Are some mums more prone to Postpartum Depression?
According to WHO, worldwide about 10 per cent of pregnant women and 13 per cent of women who have just given birth experience a mental disorder, primarily depression. Some individuals are more predisposed to developing PPD and this is generally influenced by a combination of various factors.
For example, if a woman has a family history of mood disorders or suffered depressive episodes before becoming pregnant. If she has unresolved childhood trauma, relationship issues, etc., then the risk is significantly higher. Another common factor is when the pregnancy was not planned.
However, when the mother has a healthy environment, free of external stressors, and good family support, she can navigate through PPD with more ease than other women who don’t have the support.
If a mum suffered from PPD with her first child, is it likely to recur with subsequent births?
Yes, there is a higher risk of PPD if a woman has previously experienced PPD. I believe one of the main reasons is that it becomes psychologically challenging, because the anticipation of having another episode adds to anxiety and depression while going through pregnancies.
However, not all women who have had PPD with one child will necessarily experience it again with subsequent pregnancies. Taking proactive measures for early intervention, creating a strong social and family network, and access to mental health support can minimise the risk.

Can Postpartum Depression be prevented?
It’s not always possible to prevent the onset of PPD. Thus, it is important to arm yourself with PPD awareness and preparation on how to cope during pregnancy. I developed a strategy called COPE that can be useful for couples to get started with.
Connect – Create a good network to connect with family, friends or support groups for help and support.
Open communication – Be open to expressing your thoughts, feelings, and concerns with your partner or healthcare provider. Healthy communication helps in building healthy relationships.
Prioritise – Self-care can make a positive impact on your mental health. It is vital to prioritise your personal well-being by getting enough rest, eating a balanced diet, and engaging in physical activity (with your healthcare provider’s approval).
Emotional support – Emotional well-being is key to managing stress and coping with challenges. If you have a history of poor emotional regulation, depression or other mental health issues, consider seeking professional help early. A counsellor can help you develop strategies and a support plan long before potential symptoms surface.
(See also: DEPRESSION IN CHILDREN: SPOT THE SIGNS AND SEEK HELP NOW)
Symptoms of Postpartum Depression
Early symptoms of PPD can vary among individuals and are exhibited emotionally, physically, and socially. Some common symptoms are:
- Feeling persistently sad, low, or hopeless for an extended period
- Excessive anxiety, especially about the baby’s well-being
- Headaches, unexplained pain, extreme physical fatigue or lacking energy even after adequate sleep
- Changes in appetite leading to unintended weight loss or gain
- Avoiding social interactions and withdrawing from friends and family
- Lack of motivation or interest in activities that were once enjoyable
If these symptoms persist for more than two weeks and significantly interfere with daily functioning, or the ability to care for oneself and the baby, please seek professional help.

Treatment for Postpartum Depression
PPD can have significant and lasting effects on the individual, as well as on their family and the baby, if not addressed in a timely manner. The impact can be cumulative and recurrence of ongoing mental health issues like long-term depression and anxiety disorders may result.
It is important to understand that treatment or recovery may take time, but finding the right combination of treatments and coping strategies is key. Besides the COPE strategy, some avenues of help include:
- Counselling – Professional therapy to help understand feelings, process negative thought patterns, and learn coping strategies
- Medication – A healthcare provider may prescribe medications such as antidepressants to help regulate brain chemistry and reduce symptoms
- Self-care Practices – Exercise, adequate rest, healthy eating, mindfulness, and relaxation techniques can help reduce stress and alleviate its impact on mental health
Four undergraduates from Nanyang Technological University’s Wee Kim Wee School of Communication and Information recently launched Beyond Baby Blues, aiming to enhance the well-being of mothers going through PPD by providing them with the tools and confidence to manage it. Learn more at beyondbbsg.carrd.co.
How can I help someone with Postpartum Depression?
Support from partners, family, and friends plays a significant role in the recovery process. Here is what you should do and should not do. I created these acronyms to help my clients — show CARE and do not PUSH!
Show CARE!
Calm – Maintaining a calm presence in the face of someone’s pain can offer reassurance and stability. It involves staying composed, providing a sense of serenity, and ensuring a safe, peaceful environment to help alleviate their distress and anxiety.
Attention – Giving focused attention demonstrates care by actively listening, being present, and showing genuine interest in their needs. Attentiveness involves acknowledging their emotions, concerns, and needs without distraction, providing a supportive and validating environment.
Respect – Respecting their feelings, opinions, and boundaries while they’re in pain is crucial. Showing consideration for their dignity and autonomy fosters a supportive and validating atmosphere, letting them feel acknowledged and valued.
Empathy – Empathy involves understanding and sharing the feelings of the person in pain. By expressing empathy, you create an emotional connection, validate their experience, and demonstrate a deep understanding of their emotions, ultimately providing comfort and support during challenging times.
Do not PUSH!
Pressure – Avoid pressuring them. Allow them space and time to express themselves without feeling hurried or coerced into decisions or actions they might not be ready for.
Undermine – Do not undermine their efforts or confidence. Instead, support them by acknowledging their struggles and strengths without diminishing their autonomy.
Spiteful – Avoid being spiteful or harbouring ill will towards them. Conversely, foster an environment of empathy, understanding, and care without negativity or resentment.
Hostile – Refrain from being hostile or creating an environment that feels antagonistic. Strive instead to create a nurturing atmosphere, free from hostility or aggression, to aid their well-being.

Common Misconceptions about Postpartum Depression
Early intervention and support can significantly improve outcomes and help navigate the challenges of new motherhood more successfully. On the other hand, the lack of awareness can only compound the challenges for someone struggling with PPD. Here are some common misconceptions:
PPD is a sign of weakness: Experiencing PPD is not a sign of weakness. It’s a medical condition influenced by hormonal changes, stress, and various factors. Seeking help is a sign of strength and self-awareness.
PPD only occurs immediately after birth: PPD can manifest anytime within the first year after childbirth, not just immediately after delivery. Symptoms might develop gradually and may not be noticeable right away.
PPD is just the ‘baby blues’: Postnatal Blues is a milder and more common condition that affects many new mothers. The baby blues typically occur in the first few days to a couple of weeks after childbirth. Symptoms include mood swings, tearfulness, and feelings of sadness and irritability, but it usually resolves on its own within a couple of weeks. PPD is more severe and persistent, interfering with daily functioning.
PPD only affects women: While PPD is more commonly associated with women, men can experience it too! It’s essential to recognise that fathers can undergo similar emotional challenges after the birth of a child. The reported prevalence of Paternal PPD can range from 4 to 25 per cent. However, many men don’t seek formal help, so the actual number of cases is likely to be higher than reported.
(See also: SUPPORT FOR NEW DADS – BECAUSE THEY NEED HELP TOO!)
Final Words of Advice
As a healthcare professional who has helped treat PPD, it is important to note that not everyone’s experiences are the same. If you suspect PPD, here is some advice:
Educate Yourself: Learning about PPD can help in recognising symptoms and seeking help promptly for yourself or your loved ones.
Talk It Out: Sharing your thoughts with trusted individuals about your feelings can alleviate some of the emotional burden.
Build Support: Surround yourself with supportive and understanding people who can provide assistance and encouragement.
Self-Care: Engage in activities that bring you pleasure and relaxation. Take care of yourself physically and emotionally.
Seek Help: Early intervention is crucial. Don’t hesitate to ask for support or seek help from a healthcare professional.
Featured image: Kristina Paukshtite
All content from this article, including images, cannot be reproduced without credits or written permission from SingaporeMotherhood.
Follow us on Facebook, Instagram, and Telegram for the latest article and promotion updates.





