SingaporeMotherhood | Pregnancy
September 2019
Gestational Diabetes 101 – Are You at Risk?

In Singapore, gestational diabetes mellitus (GDM) occurs in about one in four to five pregnancies. This is according to a study published in May 2018 by the Agency for Care Effectiveness at the Ministry of Health. Many think that it’s just something that happens during some pregnancies, and will go away by itself. But it’s important to recognise that GDM doesn’t only put both mother and infant at risk in the short term. It also has the potential to severely impact their health on a lifelong basis.
The Dangers for Mum and Bub
Most women who have GDM give birth to healthy babies. However, if the rise in blood sugar levels isn’t adequately managed, it can cause complications during pregnancy, delivery and beyond. Dr Christopher Chong, an obstetrician, gynaecologist and urogynaecologist at Gleneagles Hospital, shares what these are.

- Increased risk of preeclampsia, a serious pregnancy complication. It is characterised by high blood pressure and damage to organs such as the liver and kidneys. “About 20 per cent of expectant mothers with GDM have high blood pressure during pregnancy,” says Dr Chong.
- Polyhydramnios (excessive ‘liquor’) in the water bag. This increases the risk of premature delivery as it can cause the water bag to rupture too early.
- Large babies. Excessive birth weight can result in a traumatic delivery or require an emergency C-section. Baby could sustain birth injuries or be wedged in the birth canal. “For instance, shoulder dystocia, where the foetus’ head is delivered but the shoulder is stuck,” Dr Chong explains. “This can result in foetal damage and even death.”
- Respiratory distress syndrome. Premature babies may experience respiratory distress syndrome, where they may need help breathing until their lungs mature. Infants of mothers with GDM may experience respiratory distress syndrome even if they are born full-term.
- Hypoglycaemia (low blood sugar). Infants of mothers with GDM may develop hypoglycaemia soon after birth as their insulin production is high. “This can lead to poor feeding and failure to thrive,” says Dr Chong. Severe episodes of hypoglycaemia may also cause seizures.
- Sudden infant death syndrome (SIDS). In poorly controlled and especially in cases of undiscovered GMD, sudden foetal death may occur. This can happen either before birth, or shortly after.
- Type 2 diabetes later in life. Both mother and baby are now predisposed to developing type 2 diabetes, and its associated conditions such as obesity and heart disease. Infants of mothers with GDM are also more likely to develop birth defects, and have postnatal jaundice.
(See also: Breastfeeding (in a Coma) Saved My Life)
Causes of Gestational Diabetes

Gestational diabetes is a glucose tolerance disorder that happens during pregnancy. According to Dr Chong, “the real reason is not known”. Some pregnant women simply develop an insulin resistance caused by hormones that the placenta produces. “For these women, the pregnancy hormones counteract or reduce the action of insulin. Their bodies are unable to handle the sugar load as well as before pregnancy as a result,” he explains.
It’s also common for GDM to be diagnosed or discovered in the third trimester. It makes sense, since the third trimester is when the body ups its production of placenta hormones significantly. Yet not every mum-to-be suffers from GDM. Indeed, says Dr Chong, “Different individuals respond to this phenomenon differently and thankfully most will not develop gestational diabetes.”
(See also: Pregnancy Week-by-Week Guide – Everything You Need to Know as Your Baby Bump Grows)
Who is Most Likely to Develop Gestational Diabetes?

“We cannot predict or measure the anti-insulin extent of the placenta in any pregnancy. Any mother-to-be can develop gestational diabetes,” says Dr Chong. However, some women face greater risk. For instance, you are more likely to develop GDM if you:
- Have close family members, such as parents and siblings, with Type 2 diabetes
- Are in an advanced maternal age pregnancy—35 years and older
- Were significantly overweight or obese even before you conceived
- Put on excess weight during your pregnancy
- Have prediabetes—slightly elevated blood sugar, a possible precursor to Type 2 diabetes
- Had GDM in an earlier pregnancy
- Previously delivered a baby weighing over 4kg at birth, or a stillbirth
“Living a healthy lifestyle before pregnancy, losing excess weight before conceiving, exercising and eating clean—these may help lower the risk of developing gestational diabetes,” suggests Dr Chong.
But even if the risk factors don’t apply, it could still happen to you. 36-year-old Kelly Tan used to think that GDM only happens to those who like to eat sugary foods. The mum of two girls says, “Obviously that’s not true because I don’t have a sweet tooth and drink my tea black. I am physically fit and at the lower range of my ideal BMI. And I consume a relatively healthy diet; I only take brown rice and no sugared drinks.” She had borderline GDM during both her pregnancies.
(See also: What you Need to Know about Stillbirth)
Early Detection Counts
“It is true that even if you develop gestational diabetes,” says Dr Chong, “this reverts to normal naturally in six to eight weeks post-delivery.” However, with GDM posing such a health threat to both pregnant mums and their infants, we shouldn’t take it lightly. Early detection and proper treatment of GDM can help reduce the risk of developing Type 2 diabetes later in life.
“Don’t rely on typical diabetic symptoms such as thirst and the frequency of urination,” Dr Chong warns. In Singapore, all pregnant women are offered screening for GDM with an oral glucose tolerance test. This is usually done between your 24th and 28th weeks. However, if you are assessed to be at a higher risk, your ob-gyn can do the test earlier, and repeat it at 24 to 28 weeks if the result of the first test was normal.
According to Dr Chong, “Signs to suggest a need to check for gestational diabetes include excessive weight gain in pregnancy, excessive fluid in the water bag, ultrasound scans revealing a large foetus, and recurrent sugar-positive on the routine urine dip stick test, which is usually done on each antenatal visit.”
(See also: Prenatal Scans and Tests for your Peace of Mind when Pregnant)
Treatment for Gestational Diabetes

You’re right to be concerned if you are diagnosed with GDM, but it isn’t all bad news. It’s treatable and you can do something about it.
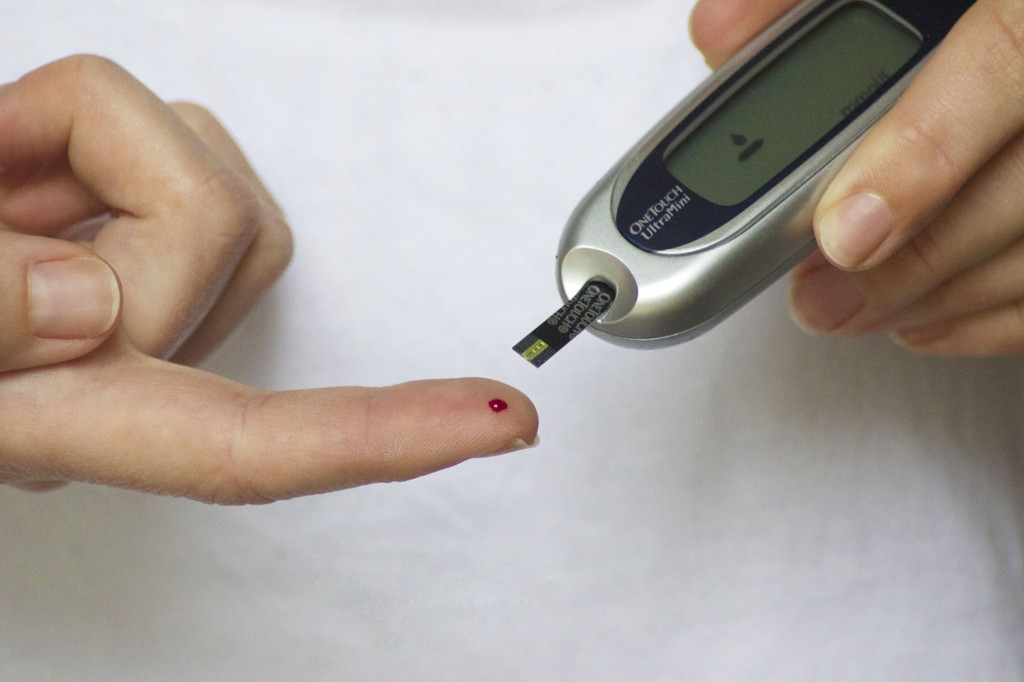
Dr Chong says, “Gestational diabetes is treated with diet control—usually restricted to 1,800 calories per day. Fasting, pre- and post-meal sugar levels are monitored by means of a hypo-count (pin-prick sugar test). If good control cannot be achieved, then we have to resort to insulin injections.”
Kelly candidly shares details of her pregnancy diet. “No fried food, no oily food, no dessert, no sugared drinks, no high-sugar fruits, no white bread, rice or noodles. My meals were mainly made up of steamed fish or braised meat, vegetables, brown rice and one slice of fruit.” She adds, “Even when I was absolutely hungry in the middle of the day, I was only entitled to a glass of milk with plain crackers!”
Tan Poh Hong, a teacher aged 40 years, is currently pregnant with her second child. She was diagnosed with GDM at Week 28. “I was referred to a diabetic specialist who gave me a device to scan my sugar level every day for two weeks. The doctor also advised me to cut back on carbohydrates and take no sugar content food stuff.” Thankfully, after following the doctor’s advice, Poh Hong’s sugar levels came under control. She no longer has to track it daily, and continues to watch her diet carefully.
(See also: Maternity Insurance: what you think you don’t need, but should have)
Looking beyond Baby’s Birth

Studies conducted by the US National Institutes of Health show that women who develop GDM during pregnancy have a significantly higher chance of developing Type 2 diabetes later in life. Their children are also predisposed to becoming obese and developing Type 2 diabetes in the future.
“My gynae was watching my weight gain closely and made sure that I didn’t gain more than 1kg per month. Even with a 1kg weight gain, I would always get an earful of nagging from him,” recalls Kelly. But she understands the concern. “I had this condition for both my pregnancies and had to monitor very closely. The baby getting overweight poses a risk of them getting diabetes in the future as well.”
If you had GDM, your doctors will check to make sure your blood sugar levels return to normal after delivery. This is usually done once right after birth, and again six weeks later. It may also be a good idea to have it checked regularly going forward, just in case.
Kelly remembers that both her babies had to be tested for high blood sugar when they were born too. “Thankfully, both were fine at birth and did not require any special follow-up by the paediatrician.”
Remember, you can lower the risk of developing gestational diabetes—and Type 2 diabetes—by making healthy lifestyle choices. Stick to a healthy diet, exercise regularly, and maintain your ideal weight. Hey, consider it extra incentive to achieve that (postpartum) figure you’ve always dreamed of!
All content from this article, including images, cannot be reproduced without credits or written permission from SingaporeMotherhood.
Follow us on Facebook, Instagram, and Telegram for the latest article and promotion updates.





