SingaporeMotherhood | Parenting
October 2023
5 Ways to Protect your Child from Antimicrobial Resistance (AMR)

Imagine a world where the bacteria and bugs that make us sick no longer respond to medicines, making infections harder to treat, and increasing the risk of disease spread, severe illness, and death. This is known as antimicrobial resistance (AMR), and it is already starting to happen now. In fact, the United Nation’s (UN) Interagency Coordinating Group on Antimicrobial Resistance (IACG) predicts that by 2050, the number of deaths globally from drug-resistant infections could rise to 10 million annually, making it even more deadly than cancer (source).
Young children, whose microbiomes are still maturing, as well as the elderly, are at significant risk. In 2019, one in 5 deaths caused by AMR occurred in children under the age of five — often from previously treatable infections.
The Institute for Health Metrics and Evaluation
In the light of World AMR Awareness Week (WAAW) which is celebrated from 18 to 24 November every year, Gerald Lee from biotechnology company QIAGEN tells us why we need to know about AMR, and what we can do to help protect ourselves and our children from it.
(See also: WHAT IS ANTIBIOTIC RESISTANCE & HOW DOES THIS AFFECT MY FAMILY?)
What is antimicrobial resistance (AMR)?
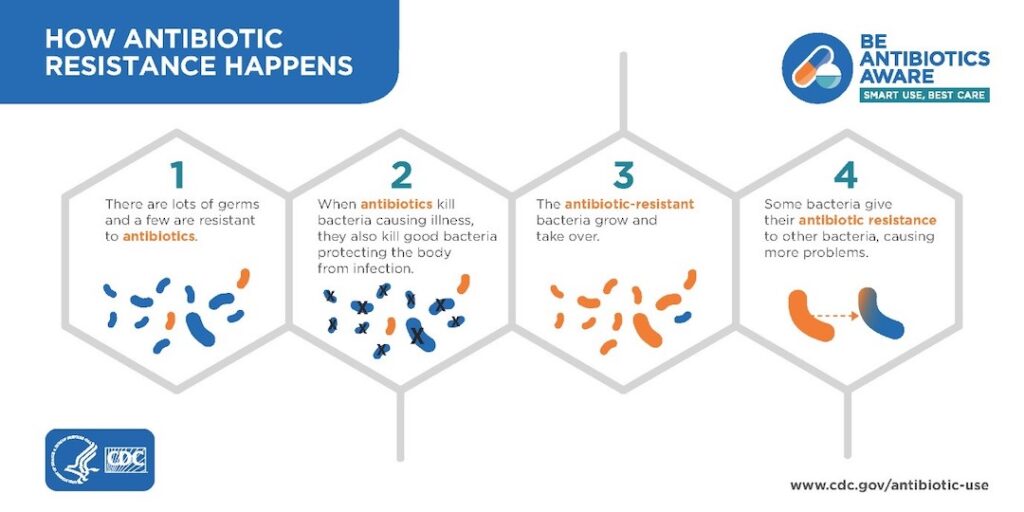
Antimicrobial resistance (AMR) occurs when bacteria, viruses, parasites, and fungi change over time and develop the ability to resist the effects of antimicrobial drugs such as antibiotics, antifungals, and antivirals. This makes infections harder to treat, and can increase the risk of more severe illness, hospitalisation, and even death.
Is AMR dangerous?
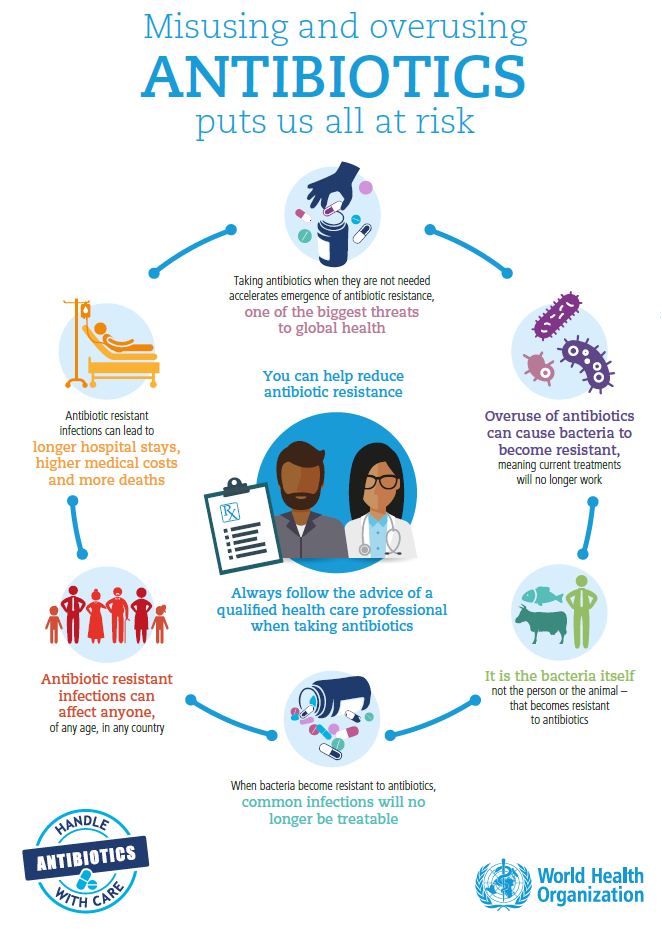
Yes. AMR is a serious threat. The World Health Organization (WHO) lists AMR among the top 10 threats to global health.
How can I explain AMR to my child?
Imagine you have a group of soldiers fighting against an enemy army. The soldiers have weapons that can kill the enemy soldiers. But if the enemy soldiers figure out how to protect themselves from the weapons, they will become resistant to the weapons.

The same thing can happen with bacteria and other microbes. When we use antibiotics, we are using weapons to kill the bacteria. But if we overuse antibiotics, or if we don’t use them correctly, the bacteria can develop resistance to the antibiotics. This means that the antibiotics will no longer be able to kill the bacteria, and the infection will become harder to treat.
(See also: INTERVIEW WITH AN ANTIBIOTIC PILL)
Where does AMR come from?
Microbes are microscopic organisms that include bacteria, viruses and fungi. Every form of life — including humans — is covered in them. Together, these microbes make up the human microbiome.
Most microbes in or on the human body are harmless and may even be beneficial. However, some microbes can cause infections and illnesses. These are known as pathogens. Over time, pathogens evolve and develop a resistance to drugs.
For example, if you do not finish a course of antibiotics for a bacterial infection, the surviving bacteria in your body can develop resistance to the drug. This leads to AMR. The same applies to other antimicrobials such as antifungals and antivirals. These are drugs that target fungi and viruses, respectively.

While antibiotics are used to kill bacteria and treat illnesses, often they do not specifically target pathogens. They can also affect other microbes and reduce the diversity of our microbiome. As a matter of fact, studies have shown that taking antibiotics decreases the diversity of our gut microbiome by at least 30 per cent.
This is not ideal as high microbial diversity ensures a healthy gut microbiome, as well as a stronger and more stable immune system. A less diverse microbiome is associated with a number of human diseases. The use, overuse and abuse of antibiotics strongly impacts our microbiome.
Keeping your microbiome healthy
As a healthy and diverse microbiome is beneficial to health, it is necessary to protect and develop it. This is especially true for young children as the human microbiome is very unstable in early life. Hence any drastic changes within may alter their microbiome permanently.
“The microbiome of a child starts developing at the moment of birth — a child delivered vaginally will have a different microbiome environment compared to one delivered via C-section. As a child matures, their microbiome develops according to their environment, people and animals they interact with, and their diet, eventually stabilising as they enter adulthood. During developmental years, changes in the microbiome can have lasting impact on a child’s life as a stable adult microbiome is unlikely to change. Therefore, it is extremely important to nurture the development of a child’s microbiome,” explains Dr Justin Chai, Director, Medical Affairs at QIAGEN.
“Can’t we just produce more new and more powerful drugs to replace the ineffective ones?” you might wonder. Unfortunately, research and development of antibiotics have slowed in recent times as these drugs are not as lucrative since they are mostly used for short-term treatments.
The importance of antimicrobial stewardship
Hence, antimicrobial stewardship is important. Antimicrobial stewardship is the systematic effort to optimise the use of antimicrobials to improve outcomes for patients, while minimising the rise of antibiotic resistance.
It involves selecting the right therapy, the right dosage, the right route and duration of use, and discontinuing the antibiotic when it has served its purpose.
In Singapore, awareness of antimicrobial stewardship is growing. Singapore General Hospital has an Antimicrobial Stewardship Unit (ASU) that works with doctors to select the most appropriate antibiotic for a patient’s medical condition, and ensure that it is optimally-dosed, and cost-effective.
To use antibiotics most efficiently, doctors have to accurately and rapidly identify the microbe that is causing symptoms. This is where fast diagnostic testing can potentially interface into antimicrobial stewardship programs to help providers determine exactly what pathogen is causing the infection, and select the most appropriate antibiotic. This improves the time to effective antimicrobial therapy, reducing unnecessary treatments and shortening length of hospital stays.
5 ways parents can play a part in antimicrobial stewardship

As parents, we too, have a part to play in antimicrobial stewardship. Here are 5 things we can do to help protect ourselves, and our children, from the threat of AMR.
1. When seeing a doctor, ask about the risks and benefits of antibiotics (as some antibiotics may have side effects), and consider other ways to treat illness.
2. If antibiotics are prescribed, ensure that your child finishes the full course, even if your child is feeling better. Not doing so may cause the surviving pathogens to build resistance against the medication.
3. Always keep antibiotics out of reach of children to prevent mis-dosing.
4. Only give your children antimicrobial drugs that are prescribed by a doctor. Do not use over-the-counter antimicrobial drugs without first consulting a doctor.
5. Get your children vaccinated to protect them from various infectious diseases. This helps to reduce the scenarios where antimicrobial drugs are required.
In addition, parents can also advocate for policies and programmes that promote the appropriate use of antimicrobial drugs. This can help to reduce the development and spread of AMR. AMR is a serious threat to health, but we can all do our part to help protect ourselves and our children from it.
Find out more about AMR, antimicrobial stewardship, and how clinicians are tackling this issue, through a podcast 30 November at 12pm. Register here.
Watch The Antibiotic Tales animated comic by Sonny Liew and Associate Professor Hsu Li Yang to learn how you can help to reduce the spread of antimicrobial resistance. Click here to watch.
Featured image: World AMR Awareness Week Toolkit
All content from this article, including images, cannot be reproduced without credits or written permission from SingaporeMotherhood.
Follow us on Facebook, Instagram, and Telegram for the latest article and promotion updates.





