SingaporeMotherhood | Parenting
May 2024
Cervical Cancer Q&A: 20 Questions Every Woman Should Ask

In Singapore, cervical cancer is the 10th most common cancer in women. That translates to over 200 new cases surfacing each year. In 2022, the National Population Health Survey reported that despite 89.9 per cent of women being aware of the Pap smear and 54.6 per cent of the HPV test, only 43.1 per cent had actually undergone a cervical cancer screening in recent years.
Yet according to medical oncologist Dr Lee Guek Eng, cervical cancer is highly preventable. In fact, the World Health Organization (WHO) wants to eliminate it by 2120 — but we need to play our part. Dr Lee, who is also a senior consultant and director for the Young Women’s Cancer Program at Icon Cancer Centre, answers 20 questions about cervical cancer and how every female can avoid getting it.
1. What is cervical cancer?
Cervical cancer is the growth of abnormal cells in the lining of the cervix. The cervix is the lower, narrow end of the uterus (womb) that connects to the vagina (birth canal). They are part of the female reproductive system, which also includes the fallopian tubes, ovaries, and vulva (external genitals).
2. Is it hereditary?
Although not hereditary, genetic factors can increase risk, particularly if an immediate family member has the disease. Furthermore, it’s very rare for women under 25 years to develop cervical cancer, with the risk increasing as you age.
(See also: CERVICAL CANCER SURVIVOR SAYS ART & HER CHILD KEPT HER ALIVE)
3. What causes cervical cancer?
Infection with Human Papillomavirus (HPV) is the most common cause or risk factor for cervical cancer. These viruses can be transmitted during sexual intercourse, including via oral or anal sex. Almost all cases of cervical cancer are caused by persistent infection with some high-risk types of HPV.

4. If I test positive for HPV, does that mean I’ll develop cervical cancer?
Genital HPV infects around eight in 10 women at some point in their lives. Yet most women who have the HPV infection never get cervical cancer. That’s because our immune systems help rid the body of HPV, just like with the any flu or stomach virus. Therefore, women with a weakened immune system (due to HIV or cancer treatments, for example) are at higher risk.
5. Since my spouse and I are faithful to each other, I can’t get cervical cancer, right?
It’s a misconception that you can’t get cervical cancer if you have only one sexual partner. While multiple sexual partners increase the risk through an increased chance of HPV exposure, it is important to note that there are other risk factors at play.
6. So what are some other risk factors?
Besides having multiple sexual partners, other factors that increase your risk of cervical cancer include becoming sexually active at a young age and having a partner who is considered high risk. Smoking — and passive smoking — is another. Chemicals in tobacco can damage the cells of the cervix, making cancer more likely to develop in women with HPV.
(See also: AFTER ALMOST 10 YEARS OF PAINFUL INTERCOURSE, THIS MUM-OF-TWO LEARNT SHE HAD PEVD)
7. What about contraceptive pills?
Research shows that women who have taken oral contraceptives (‘the pill’) for five years or more are at increased risk of developing cervical cancer. The reason for this is not clear. However, the risk is small and the pill can also help protect against other types of cancer, such as uterine and ovarian cancers.
8. Can I still develop cervical cancer if I remove my reproductive organs?
Yes, cervical cancer can still develop even after undergoing a full hysterectomy to remove your uterus. This can happen when cervical cancer cells had already spread to other organs before the procedure. In a partial hysterectomy, the cervix is left intact, hence developing cervical cancer afterwards is still possible.
9. What are the early warning signs of cervical cancer?
There are usually no symptoms in its early stages. The only way to know if there are abnormal cells in the cervix is to undergo a cervical screening test.

As the cancer advances, symptoms typically include:
- Heavier period or periods that last longer than usual
- Unusual vaginal discharge
- Vaginal bleeding between periods or after menopause
- Vaginal bleeding during or after sexual intercourse
- Pain during sexual intercourse
- Pelvic pain
10. Are regular screenings really necessary?
All women aged 25 and above should go for regular screening regardless of whether you experience any of the symptoms. This is because cervical cancer is a ‘silent killer’. If you belong to a high-risk group, please consult your doctor for the recommended screening frequency and types of tests.
11. Is cervical cancer fatal?
Indeed. In fact, with about 70 deaths from cervical cancer yearly, it ranks as the 10th deadliest cancer in Singapore. Early detection is key, as survival rates from 2017 to 2021 prove. They stand at 85.4% in the first year, but fall progressively to 62.8% by Year 5.
12. What are some treatment options?
Typical options include surgery, chemotherapy, and radiation therapy. For early-stage cervical cancer, you may undergo surgery to remove a small area of the cervix. For Stage 2 onwards, when cancer spreads beyond the cervix, it usually requires a combination of treatments. Immunotherapy for locally advanced and metastatic cervical cancer is the newest treatment paradigm.
13. Is cervical cancer preventable?
There are currently two ways to prevent cervical cancer. Firstly, with HPV vaccines. The full vaccination comprises three doses over a 6-month period for females between the ages of 9 and 26. Vaccine efficacy is extremely high for women yet to be exposed to HPV infections and the protection is long-lasting. Secondly, through regular screening tests to detect cells in the pre-cancerous stages.
(See also: OPT-IN HPV VACCINE FOR GIRLS IN SINGAPORE: SHOULD MY DAUGHTER GET IT?)

14. What are the various screening tests available in Singapore?
For women 25 years and above and are sexually active, Pap tests are recommended once every three years and HPV tests once every five years. They check for cervical changes and the presence of high-risk types of HPV (HPV-16 and HPV-18) respectively.
15. Are the screenings painful?
Both the Pap test and HPV test involve inserting a speculum into the vagina gently to obtain a sample of the necessary cells. There is generally some discomfort but most women find it tolerable, and it only lasts a minute or two. The sample is then sent off to the lab for testing.
16. If the test is positive for HPV, what’s the next step?
If you test positive for HPV, your doctor will conduct more diagnostic tests to determine if you are at risk of cervical cancer. This can include Pap tests and colposcopy. A colposcopy is a simple outpatient procedure that allows the specialists to take a closer look at your cervix. If they detect any abnormal cells, they may perform a biopsy for further evaluation.
17. Does being HPV-positive affect my chances of conception?
An HPV infection itself is unlikely to affect fertility outcomes directly. However, if the infection leads to complications, some treatments might have an impact on fertility. Please consult your doctor for a detailed discussion.
(See also: I DREAM OF GYNAE – HOW TO CHOOSE DR RIGHT WHEN YOU’RE PREGNANT)
18. Does an HPV infection endanger my pregnancy in any way?
HPV infections don’t usually pose a direct threat to pregnancy. However, in cases where genital warts or lesions are present, there might be a slightly increased risk of complications like preterm birth.
19. If I and/or my spouse are HPV-positive, can we pass it to our unborn child?
Although this is rare, it is possible for the infant to contract HPV during vaginal delivery if the mother has active genital warts or lesions. But not to worry. In most cases, your newborn’s immune system will clear the infection in due course.
20. Where can I get my Pap or HPV test?
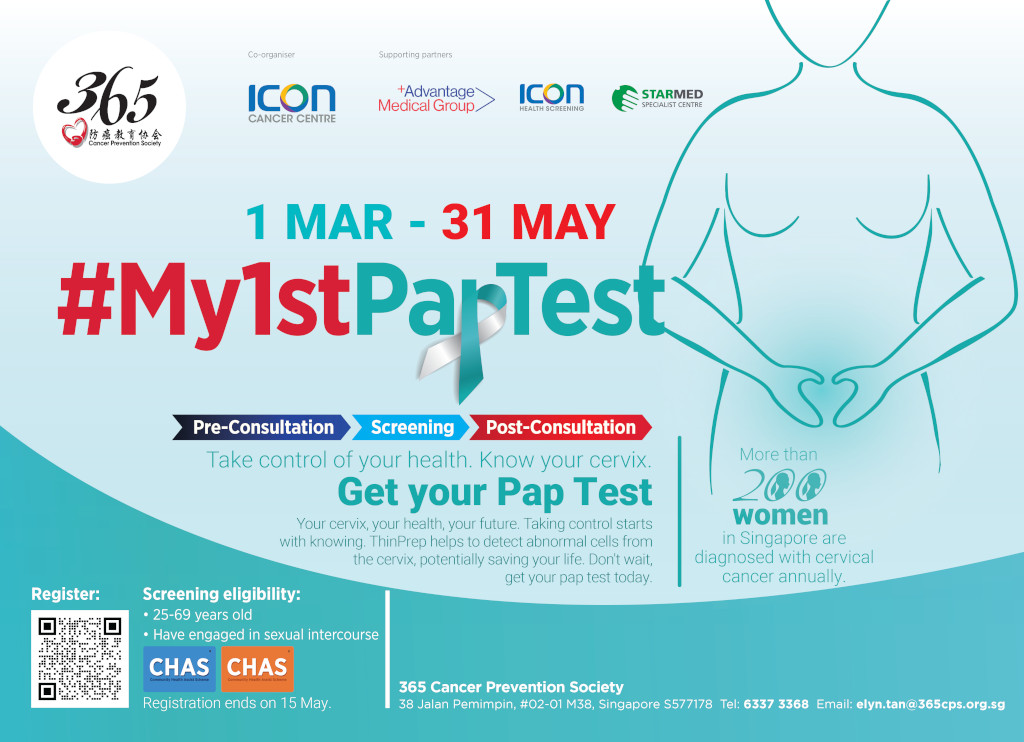
Together with Icon Cancer Centre, 365 Cancer Prevention Society (365CPS) is running its inaugural #My1stPapTest campaign for lower-income Singaporeans. If you are between 25 and 69 years old, and have a valid blue or orange CHAS card, register for your free ThinPrep Pap Test by 15 May 2024.
Otherwise, Singapore citizens are eligible for subsidised health screenings at GP clinics under the national Screen for Life programme.
Members of the public who wish to support #My1stPapTest can do so via Giving.sg or Give.asia. All donations to 365CPS are eligible for 250 per cent tax relief.
(See also: MAMMOGRAMS IN SINGAPORE – SUBSIDISED BREAST CANCER SCREENING PROGRAMMES & COSTS)
Featured image: freepik. All other images courtesy of 365 Cancer Prevention Society
All content from this article, including images, cannot be reproduced without credits or written permission from SingaporeMotherhood.
Follow us on Facebook, Instagram, and Telegram for the latest article and promotion updates.





