Angelica Cheng
Active Member
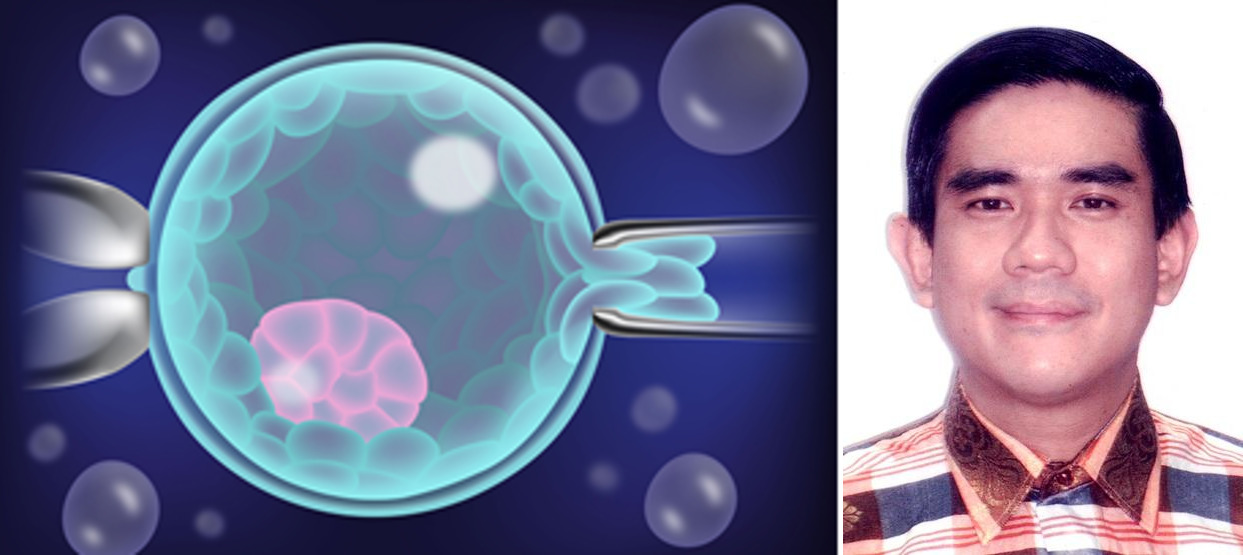
"IVF genetic testing to prevent birth defects in older women"
In conversation with Dr. Alexis Heng Boon Chin, Associate Professor, Peking University, China
With an increasing trend of late motherhood, many women across Asia and worldwide are choosing to postpone childbearing while prioritizing lifestyle and career objectives. Nevertheless, the risks of conceiving a baby with genetic (chromosomal) abnormalities increase with older maternal age, the most common and well-known of which is Down syndrome. Worldwide, more than 90% of Down syndrome fetuses are routinely aborted upon positive diagnosis by prenatal testing. However, there are serious risks to the mental, physical and reproductive health of the patient to consider, when aborting a fetus diagnosed with Down syndrome or other genetic abnormalities.
For older women undergoing assisted reproduction treatment, there is a way of avoiding this abortion quagmire by genetic screening of IVF embryos before transferring into the womb, a highly expensive procedure known as Preimplantation Genetic Testing - Aneuploidy (PGT-A) or Preimplantation Genetic Screening (PGS). Hence, the pertinent question that arises for older women undergoing assisted reproduction treatment, is whether it is worthwhile and cost-effective to utilize expensive PGT-A (PGS) for screening and excluding genetically abnormal embryos, as compared to standard prenatal testing techniques that are much cheaper.
What are the different types of genetic abnormalities that occur in older mothers?
Due to a lack of proper separation of chromosomes during egg development in older women, they are at higher risks of genetically abnormal births.
The most common genetic abnormality in older mothers is Down syndrome, caused by an extra copy of chromosome 21. Additionally, increasing maternal age is also associated with elevated risks of Edwards syndrome (extra copy of chromosome 18), Patau syndrome (extra copy of chromosome 13) and Klinefelter syndrome (extra X chromosome - 47,XXY). Among these, only babies with Down and Klinefelter syndromes usually survive to adulthood. The life expectancy of Patau syndrome is around 7-10 days, with 90% dying in the first year of life.
Similarly, the average lifespan for Edwards syndrome is 3 days to 2 weeks, with only 5% to 10% of afflicted infants surviving for over a year. Down syndrome is characterized by a substantial reduction in lifespan to about 60 years, severe impairment of mental and physical development, together with increased predisposition to certain medical conditions such as congenital heart defects, type II diabetes and Alzheimer’s disease (after the age of 40). In contrast, for Klinefelter syndrome (47, XXY), there is only a very slight reduction in lifespan by about 2 years compared to the normal male population (46, XY). Although individuals with Klinefelter syndrome usually have normal intelligence, they suffer from infertility and have small underdeveloped male sex organs, poor motor coordination and weak muscles, reduced facial and body hair, breast growth, and low sex-drive.
According to published medical statistics, the risks of conceiving a genetically abnormal baby for women in their late 30's, around 37 to 39 years old, is approximately within the 0.8% to 1.2% range. By age 40, the risk of genetic abnormalities increases to about 1.5%, and then to around 4.8% at age 45.
Can genetic testing potentially harm IVF embryos?
IVF genetic testing involve drilling a hole through the embryo shell (Zona Pellucida) and extracting cells from the embryo, which is potentially harmful, and can impair it’s development. Experts have pointed out that studies claiming no ill effects to embryos are often based on PGS of excellent-quality, healthy, robust embryos rather than more “delicate” embryos that might suffer more. If you have just one or two embryos, you might decide it is not worth the risk. No matter how well-trained is the lab staff (embryologist) doing this procedure, there is still a risk of human error. The more busy the IVF lab is, the greater the risk of human error, as lab staff are under pressure to complete procedures as fast as possible.
What are the challenges associated with IVF genetic testing?
There are several aspects to be considered towards genetic testing in IVF treatment.
- IVF genetic testing involve extracting and sampling cells from the outer embryo layer that gives rise to the placenta and umbilical cord. This is not representative of the inner embryo layer that goes on to form the actual embryo proper, which gives rise to the baby.
- Mosaic embryos, which are embryos with a mixture of genetically normal and abnormal cells occur quite frequently and commonly among woman undergoing IVF. Genetic testing often leads to the misdiagnosis and discarding of mosaic embryos, which have been shown to be capable of giving rise to a normal and healthy baby. Recently in 2020, a class-action lawsuit was filed by Australian patients against misdiagnosis by IVF genetic testing, which led to discarding of their viable embryos and consequent loss of chance at parenthood.
- There is scientific evidence that Mosaic embryos are able to “self-correct”, which increases the chances of normal birth. This “self-correction” mechanism involve pushing out the genetically abnormal cells into the outer embryo layer, which gives rise to the placenta and umbilical cord.
- Older women with low ovarian reserves have much fewer embryos during IVF. Therefore excluding or discarding of mosaic embryos that can potentially give rise to a normal baby, would in fact substantially reduce their chances of IVF success. Some older women may have no embryos left to transfer after genetic testing.
Are there alternative methods to IVF genetic testing for preventing birth defects in older women?
Yes, there is an alternative method that is much cheaper than PGT-A (PGS). This is known as Non-Invasive Prenatal Testing (NIPT), in which the DNA of fetal cells within the expectant mother’s blood circulation is extracted and tested for genetic abnormalities. Nevertheless, the downside is that NIPT can only be performed after getting pregnant, so the patient has to be mentally and emotionally prepared to abort a genetically abnormal fetus. Additionally, ultrasound can also be used to some extent for detecting Down syndrome, even though the results are not as accurate and determinative as NIPT.
How cost-effective is IVF genetic testing for older women?
Given the uncertain outcome and high costs of IVF treatment, it may be preferable for some patients with limited funds to cut costs by not doing genetic testing, so as to save money for future attempts at IVF treatment, given that cheaper alternative prenatal testing methods are available. After all, more than one IVF attempt is usually needed to achieve reproductive success, and it would be financially exhausting to do genetic testing for each and every IVF treatment cycle. As mentioned earlier, given that the risks of genetic abnormalities do not exceed 5% for almost the entire female reproductive lifespan (20 to 45 years old), it may be highly cost-inefficient to utilize such an expensive procedure for all older women undergoing IVF, In particular, the incidence of genetic abnormalities is typically less than 1.5% for women below 40 years old, so that utilizing PGT-A would be superfluous more than 98.5% of the time. Ultimately, it is up to patients with limited financial resources to decide whether it is worthwhile taking a calculated risk of avoiding highly expensive genetic testing, to get more shots at IVF.
Can you elaborate on the principles and regulations of IVF genetic testing in Singapore?
Singapore healthcare policies allow IVF genetic testing only for mainstream clinical treatment for patients who are sufferers or carriers of known genetic diseases (PGT-M & PGT-SR). Routine genetic screening of IVF embryos of older women (PGS or PGT-A), who are at increased risks of Down syndrome is still not approved as mainstream clinical treatment but is restricted to a tightly regulated clinical trial at government hospitals. To participate in this clinical trial, women have to be 35 years old or older, or have suffered two recurrent miscarriages, or have two failed IVF attempts. Also, there are inadequate and doubtful results from the current clinical trial of IVF genetic testing in Singapore, which was reported to suffer from a high attrition rate of 72%.
Last edited: